Dr Lee Humber
Author of Vital Signs:the Deadly Costs of Health Inequality.
As the world continues in lockdown, and governments fumble for ways of getting us out and back to work, questions remain about how well our long term health regimes prepare us for and protect us against the possibility of a continued era of epidemics. Here, I look at how our health relates to the environments we live in, and at how models of health enable – or disable – us as we face the new, evolving conditions of life implicit in concepts of the Anthropocene.
If large-scale environmental changes occur, such as climate change, land degradation and biodiversity loss, then we must expect that the life-supporting capacity of the biosphere will diminish. For example, such changes will alter the geographical range of, and the pattern of human contact with, various infectious diseases. They will also affect the productivity of agroecosystems, especially in already food-insecure zones, and hence might increase regional levels of malnutrition, and disrupt local livelihoods and communities with the consequent health risks of displacement and refugee-status. (D.J. Rapport, Assessing Ecosystem Health, 1999)
Written over twenty years ago Rapport’s work made the clearest of links between climate change and human health. Focussed then on broad differences between the relatively more industrially developed Global North and the Global South, it is now clear that neoliberalism, especially following its austerity phase since 2008, has brought ‘food insecurity’ and ‘malnutrition’ to large swathes of the US and Europe, with the subsequent enfeebling of populations becoming only too visible during the COVID19 pandemic. Rapport and over the last twenty years much other research has been clear that an important effect of ecosystem degradation, indeed its personification, is an increased risk to human population health. As well as the directly toxic impact of the bioaccumulation of pollutants like, for example, mercury, lead, organocarbons and others, there are broader impacts on human population health from environmental degradation arising from ecological and social change and disruption.
Total human habitat
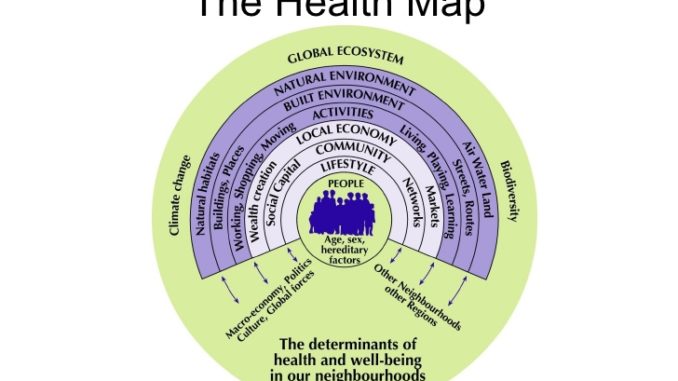
To grasp the centrality of an analysis of health to understanding the climate crisis, we need first to understand the environment as the total human habitat. Below, I critique models of health in more detail but note here that the Barton and Grant health map of 2006, provides a holistic view of the general health environment we as human organisms inhabit. The three elements of their ‘built environment’, ‘natural environment’ (which includes ‘natural habitats’ and ‘air, water, land’) and ‘global ecosystem’ (‘climate change’ and ‘biodiversity’) model is a multifaceted way of comprehending what the term ‘environment’ implies. Looked at this way, human population health should be understood as an expression of the life-supporting capacity of the total environment. Equally, population health indicates whether we are achieving a sustainable relationship with this three-pronged environment. In other words, the global population’s health reflects the extent to which the human organism’s relationship with its environment is in balance. What the pandemic clearly shows, especially when considered as the latest ill health episode in an extended era of infectious and ‘non-communicable disease’ epidemics world-wide, is that the organism-environment relationship is out of balance to such an extent as to threaten the continuation of our species. The metabolic rift, a concept developed by Marx over 150 years ago to describe the rupture between human beings and the rest of nature resulting from the onset of industrial capitalism, is without doubt widening. This situation has arisen not because of some general tendency towards over-consumption by a bloated global population as some argue, but very specifically because capitalism can only survive by exploiting the world’s resources for profit to the detriment of all else.
Human-induced changes in the Earth’s systems, including its ecosystems, have been evident since industrial capitalism evolved as the dominant mode of production through the 19th century. However, the pace and magnitude of anthropogenic change increased sharply after 1950, with that decade marking the beginning of ‘the Great Acceleration’ in the human transformation of the global environment. Among the many global indicators of accelerating change are increases in atmospheric CO2 and surface temperature, ocean acidification, deforestation and agricultural intensification, loss of biodiversity and oceanic ecosystems which in turn are triggering rapid ecosystem changes. Together, these markers of what is known as environmental stress show that capitalist modification of environmental conditions is moving the Earth beyond the stable environmental boundaries of the Holocene epoch in which human societies have been able to grow and prosper to a new ‘human-dominated geological epoch’, the Anthropocene. Many of Earth’s systems have entered ecologically a-typical states, posing unparallelled threats to human health, disproportionatelyeffecting poorer communities who have contributed least to environmental and climate change.
Though far from perfect, the Barton and Grant model is a useful way of conceptualising the interlinking nature of human health and environment so long as we understand it in the context of the dialectical relationships it implies. As the Marxist biologists Lewontin and Levins show, ‘there is no organism without an environment, but there is no environment without an organism…environments are as much the product of organisms as organisms are of environments’. Each element in the model must be understood, therefore, as both causative and caused. Looked at this way we can understand how changes at one level can impact onanother in reciprocal, bi-directional ways. This is the core of the value of what has become known as the social determinant of health approach. With its focus on how health is governed by social environments – which as the above has shown are themselves inextricably interlinked with ecological and ‘natural’ ones – the model provides a tool for understanding how changes at the level of living and working conditions and, importantly, at the level of wider economic systems themselves, determine not simply human health, nor only human society but can impact at the level of global ecosystems. Put simply, this means the fight for better conditions of work is the fight for better population health is the fight for a more sustainable and health-supporting relationship with global ecosystems.
Over the last decade by insisting on the social linkages in global health the social determinants of health approach has established itself as the key means of understanding – and potentially making an impact upon – global health and global health patterns. In the process too – and perhaps inadvertently – it has shone an all-too-bright light on the inadequacies of, in particular, the biomedical model of health which has dominated individual and population health debate as I discuss below.
The social determinants of health (SDH) are a combination of social, economic and political factors that shape the health and long-term health experiences of individuals, communities and populations. It is a modern form of an analysis of population health developed in the mid 19th century by Frederick Engels. In his landmark The Condition of the Working Class in England Engels establishes that the ill health and short life expectancies of the workers of the rapidly expanding industrial towns of England were utterly conditioned by the poor diets, poor accommodation and lack of rest and recovery which was – and largely remains – endemic to industrial capitalism. Nearly two centuries later, the World Health Organisation said in its 2008 keynote publication, Closing the Gap in a Generation, the, ‘[U]nequal distribution of health-damaging experiences is not in any sense a “natural” phenomenon but is the result of a toxic combination of poor social policies, unfair economic arrangements and bad politics.’
For the WHO and other international health bodies, there are therefore two broad areas in need of attention to improve global health. The first are our daily living conditions, including healthy physical environments, fair employment and decent work, social protection across the lifespan and access to good quality healthcare. The second major area concerns the distribution of power, money and resources, including providing a sense of social and political empowerment, equity in health programmes and public financing of action on economic inequalities. The Rio Political Declaration on SDH which followed in 2011 noted that health inequities arise from the ‘societal conditions in which people are born, grow, live, work and age, including early childhood development, education, economic status, employment and decent work, housing environment and effective prevention and treatment of health problems.’ In 2018, a further report by WHO placed this approach in the context of environmental degeneration showing that polluted air alone – at the interface of natural and built environments – is having a devastating impact on billions of children around the world leading to hundreds of thousands of deaths. The study found that more than 90 per cent of the world’s young people – 1.8 billion children – are breathing toxic air, storing up a public health time bomb for the next generation. The report points to the scale of the crisis in both rich and poor countries – from low birth weight to poor neurodevelopment, asthma to heart disease. This social and environmental understanding of health presents a powerful and widely accepted conceptual model for action driven by a modern form of preventative, global public health engagement.
Neo-liberalism and public health
As readers may know, exactly the opposite has occurred with those public health services which remain public savagely cut back – £860 million cut from UK services over the last three years; $15 billion cut from services in the US since 2018 – while the last twenty years has seen a global shift towards private healthcare and an increasing concentration of health capital into fewer, larger corporations. As the pandemic hit, what has become known as the industrial-medical-complex, a precariously joined collection of major chemical-pharmaceutical producers and retailers, health insurance companies, the higher echelons of the medical profession and governments of leading economic powers, has never been as profitable or as powerful. Wedded to a biomedical model of health which focuses on curative practice and interventions, the industrial-medical-complex was completely unprepared for the pandemic and remains powerless to do anything about it until a vaccine is found. Looking to the future, as industrial agricultural practices continue to release new pathogens into our environment it will always be the case that the curative approach central to the biomedical model will always be chasing new virus strains after the fact. Meanwhile, while the world waits for this uneasy industrial-scientific alliance to develop a profitable cure for COVID-19, hundreds of thousands die. Though the concepts underpinning the biomedical model evolved from the late 19th century onwards, in practice it has only had a mass impact in the post WWII era. For Roy Porter, in his epic history of medicine, The Greatest Benefit to Mankind, ‘In the UK…it was only when the state began to underwrite general practice following the 1911 National insurance Act and, especially, the National Health Service after 1948’ that biomedicine made an impact on the majority of the population. Through links with successive governments globally, the biomedical model has become embedded in the modern, state and private institutions of health.
The bio–medical model and health capital
Despite all evidence showing health results from our relationship with our environment the biomedical model continues to dominate, overwhelmingly concentrating resources on funding for hospitals and medical research, on medical techniques and technologies. (For an illustration of this, we need look no further than the research money currently being thrown at the hunt for a vaccine – from which the industrial-medical-complex will profit – in comparison with what little attention is being paid to future provisioning of public health provision to avoid future epidemic outbreaks). Public discussion about health have been dominated by biomedical models that have confined debate to one centred on an individual’s relationship with natural disease, ameliorated by the expertise of the medical profession in partnership with the state. Set against the relational models explained above, the biomedical model is based on an understanding of health as the absence of biological abnormality where diseases have specific, and largely unchanging biological causes identified and known to the medical profession. The human body is regarded as a machine to be restored to health through personalised treatments that arrest or reverse the disease process, irrespective of the social conditions in which patients live, abstracting health out of its determining environment. Resulting from this approach, the health of a society is dependent on the level of medical knowledge and the availability of medical resources. This is an historical fallacy. Medical advance has always lagged behind population health improvements, as Thomas McKeown first showed as long ago as 1976 and has been consistently and conclusively shown, and widely accepted, ever since. Medical and scientific advance is important, of course, but as only one among many social determinants of health. It has never been sufficient to improve general health outcomes across populations. For that, preventative health-related measures, for example, good standards of sanitation, housing, diet and employment practices and more at broader levels, are required.
It is absolutely clear that the biomedical model serves the interests of health capital. So-called ‘Big Pharma’ pockets trillions every year on the premise that our health is underpinned by drugs and the expertise of the medical profession providing cures when we fall ill. Big Pharma’s monopoly grip on drugs pricing is a widely recognised scandal, inflating the prices of often vital drug treatments, at times even to the point of being beyond the financial reach of their customers, non-sensical even within their own terms.Health companies are amongst the most profitable companies in the world, with three health companies in the top 10 profit generators in the US alone. However, the model also serves an important ideological purpose for the capitalist class generally in that it helps turn human health into a commodity. Through a process of what Marxists term reification, health becomes a thing that we need to buy in order to avoid ill health and the poverty, and downward spiral of greater ill health and social exclusion that entails.
As the Hungarian revolutionary socialist Gyorgy Lukacs explained, reification turns the human relationship with material objects upside down so that objects are transformed into subjects and subjects are turned into objects. The result of this is that subjects are rendered passive and determined, while objects are rendered as the active, determining factor. In the case of health, concepts of health as encapsulated in biomedical models become the active object while the passive subjects are you and I. We are subject to a determining concept of health, which we must strive to possess – by changing our ‘health behaviours’ to those prescribed for us and buying the right drugs – or face the material consequences of ill-health and disease.
Objectively a world of objects and relations between things springs into being…The laws governing these objects are indeed gradually discovered by man, but even so they confront him as invisible forces that generate their own power…Subjectively…a man’s activity becomes estranged from himself, it turns into a commodity which, subject to the non-human objectivity of the natural laws of society, must go its own way independently of man just like any consumer article. (Lukacs, History and Class Consciousness, 1923)
So, our human capacity to be healthy, to make empowered choices about what is and isn’t good for our survival – an organism’s understanding of how to manage its own relationship with its environment – is alienated from us and our health becomes the property of an objective ‘health’ commodity, possessed by the industrial-medical-complex, for sale. The biomedical model will retain its hegemonic position until the institutions of health in which it is embedded are dismantled and new, preventative models of health based on expanded and more thoroughly dialectical SDH approaches take shape. The work of dismantling this is intimately tied in with the broader task of ending an economic system based on the anarchic pursuit of profit above all else and replacing that with a democratic, planned and egalitarian socialist society based on need – not profit.

This is a very useful article,